Why do you need a retainer to keep teeth straight after having braces?
The answer……….muscles!
Orofacial myology, otherwise known as myofunctional therapy, is a specialised field looking at the muscles of the face, mouth, throat, and jaw. Just like all other muscles, these need to be re-trained when imbalanced. An orofacial myologist may be required to assist in providing care for conditions like TMJ dysfunction, mouth breathing, snoring/sleep disordered breathing, crowding of the teeth/malocclusion, speech issues, non-nutritive oral habits (like thumb sucking or prolonged dummy use) and tongue ties. This is usually done alongside other practitioners like an ENT specialist, dentist, or speech pathologist.
Whatever the initial cause, when muscular imbalance occurs to muscles in and around the face, it can prompt ongoing problems with occlusion (alignment of the teeth), swallowing, chewing, speech (eg. a lisp), sleep disordered breathing, TMJ dysfunction, and palate and jaw growth.
The study of orofacial myology is a small but growing field, becoming more recognised among dentists, orthodontists and ENT specialists. Practitioners studying orofacial myology must be an AHPRA registered practitioner, and tend to be in the dental, speech pathology and musculoskeletal fields (like chiropractors).
Mouth Breathing
Mouth breathing at rest both during the day and at night is an issue. We were never designed to breathe through our mouth. The nose is a much more efficient filter of inhaled air. It is designed not only to reduce unwanted particles from entering the respiratory system, but to warm and humidify the air via the built-in turbinates in the nasal cavity. Breathing through the mouth means other structures may be overwhelmed, dealing with foreign particles in the inhaled air. Mouth breathing also means that the tongue must be positioned on the floor of the mouth to allow air in. This is particularly important in children. Without the tongue resting on the roof of the mouth, impairing proper function, there is a greater risk of underdevelopment of the upper jaw, resulting in crowding of the teeth. This may also impact optimal development of the nasal cavity, as the roof of the mouth is the floor of the nasal cavity. Development of the lower jaw is governed by the upper jaw and under development may lead to crowding of the lower dentition. This can lead to increased pressure on the TMJ (jaw joint) with recession of the lower jaw. All these changes can also impact the muscles of the face and neck with tendency toward a recessed chin, elongated face, enlarged nose and hunched posture. Abnormal posture can increase the tendency towards musculoskeletal pain like headaches and neck pain.
Another important aspect is nitric oxide. The sinuses produce nitric oxide, a powerful substance that helps fight off opportunistic microbes and enhances oxygen and carbon dioxide exchange in the lungs. Nitric oxide also stimulates the production of vasopressin, a substance that helps supress urine production during the night. Breathing through the nose transports the nitric oxide form the sinuses. With this, it’s easy to understand some of the symptoms mouth breathers may exhibit including dry lips, increased urination during the night, tiredness, moodiness and crowding of the teeth.
In mouth breathers, it is important to get to the cause. Mouth breathing can be due to the inability to breathe through the nose or the inability to keep the tongue on the roof of the mouth. Possible causes include an obstructed nasal passage (such as congestion from allergies, deviated septum, enlarged turbinates), enlarged tonsils and adenoids, tongue tie or oral habits such thumb and pacifier sucking. Once the root cause has been addressed, resulting muscle imbalances and dysfunction should be addressed via myofunctional therapy to restore function.
SLEEP DISORDERED BREATHING (SDB)/SNORING
Sleep disordered breathing, sleep apnoea and snoring all indicate some form of obstruction in the airway. This can be due to enlarged adenoids and tonsils, an underdeveloped airway, genetic factors, low muscle tone of the pharynx or other structural issues. The primary concern is that all the above most likely result in reduced oxygen levels at night. There have been established links to sleep disordered breathing in children with ADHD symptoms and behavioural issues. In adults there have been links to increased risk of cardiovascular disease. Considering the primary outcome is reduced oxygen at night, a time when we heal, snoring and sleep disordered breathing is not something that should be ignored.
After a consult with an ENT or sleep specialist, myofunctional therapy may be required to help re-train the body to breathe through the nose or strengthen the pharyngeal walls and associated muscles to open up the airway and keep it patent.
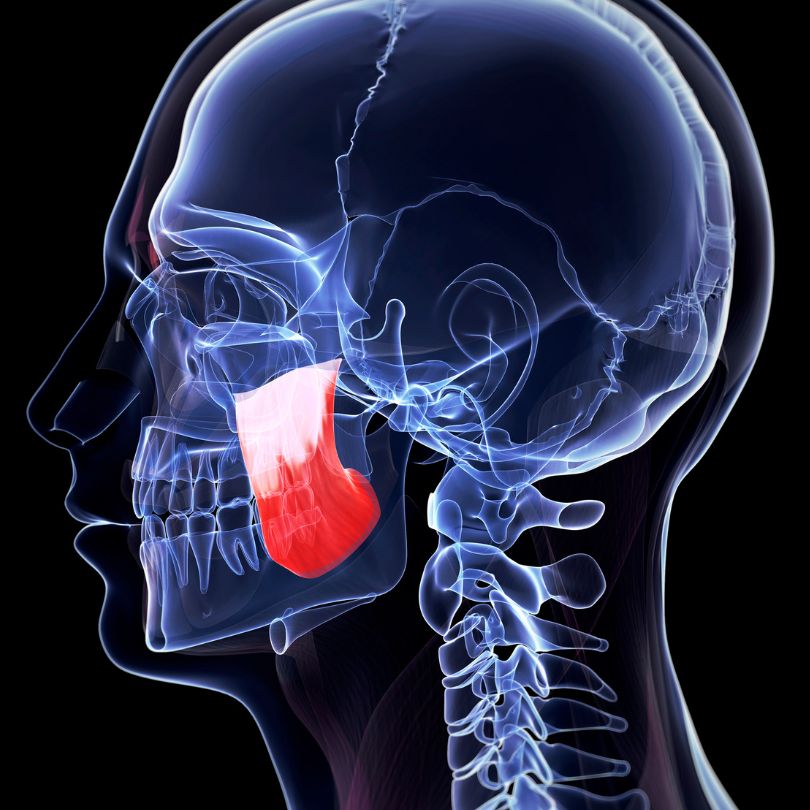
TMD (TMJ Dysfunction)
There are many causes of TMD. It is important to be assessed by someone well trained in TMD to identify possible root causes, to design a treatment plan addressing the TMD as well as any underlying conditions that may exacerbate TMD symptoms.
Myofunctional therapy can assist in addressing the muscle imbalance that occurs with the jaw muscles, as well as some of the other causes and contributing factors of TMD such as tongue position and function, reduced muscle tone of the airway (pharynx), abnormal breathing patterns and posture.

ORAL HABITS
Non-nutritive oral habits such as prolonged use of a pacifier, thumb sucking and nail and lip biting may change how the teeth sit (occlusion) and how the tongue works. This can create an imbalance and dysfunction of the muscles in and around the mouth.
Prolonged thumb sucking and/or pacifier use means the presence of the thumb or pacifier within the mouth can create an anterior open bite (where the central upper and lower teeth do not come together and form a gap). It also encourages the tongue to sit down on the floor of the mouth, which can result in mouth breathing, an underdeveloped jaw/palate and abnormal use of the tongue (which can result in speech and swallowing difficulties). Addressing cessation of the habit as well as any orofacial muscular imbalances as early as possible is important in preventing further issues with speech, swallowing, occlusion and/or nocturnal breathing.
CROWDING AND MALOCCLUSION
(Crooked Teeth)
An early sign of possible muscular imbalance within the mouth is crowding of the teeth. While genetics can be a factor in not having sufficient space for adult teeth, many cases are due to an imbalance of forces within the mouth.
Common presentations of crowding involve poor tongue posture where the tongue sits on the floor of the mouth. The altered tongue function influences the bone of the roof of the mouth to inadequately expand, reducing the size of the upper jaw and the amount of space for the upper dentition.
When the buccinator (cheek) muscles are overactive, often coinciding with the sides of the tongue being under active, the forces produced can create a cross bite, where the molars lean in towards the tongue. Overactive cheek muscles also have an association with under development of the lower jaw.

An anterior (front) open bite, where the teeth at the front of the mouth do not touch, can be produced with an anterior (forward) tongue thrust. When the tongue sits too far forward in the mouth due to lack of space or improper posture or function, the tongue may abnormally thrust forward during speech and/or swallowing, putting greater pressure on the front teeth, tilting them forward.
A tongue tie (ankyloglossia) is when the tongue is attached to the floor of the mouth by a shortened or tight frenulum. The frenulum is a normal part of the anatomy, however, when the tissue is short and restricts the movement, it is considered a tongue tie.
An anterior (front) tongue tie may be obvious, usually observed at the front of the tongue and stops upwards and forwards movement of the tongue. This may produce a dimple on the tongue where the frenulum is pulling, or the typical heart shaped tongue when the tongue is lifted.
However, there are also posterior (to the back) tongue ties. These are much harder to see and can only be diagnosed by assessing function. Ultimately, a tongue tie needs to be considered for intervention if there is restricted movement causing reduced or abnormal function. This is particularly important in infants that are unable to feed adequately due to a tongue tie. Some undetected tongue ties can increase the risk of speech and swallowing issues, sleep disordered breathing and malocclusion.
Myofunctional therapy is important in tongue tie presentations to ensure the tongue regains normal movement and function, whether a release is deemed required or not.
TONGUE TIE (ankyloglossia)
What Does The Research Say?
There is growing research indicating that orofacial myology has a definitive place in assisting in tongue thrusts, obstructive sleep apnoea (OSA), TMD, abnormal swallowing patterns, non-nutritive oral habits, malocclusion & orthodontics and tongue ties. Below are some references to start with but a search on PubMed will reveal so many more.
References
Brożek-Mądry E, Burska Z, Steć Z, Burghard M, Krzeski A. Short lingual frenulum and head-forward posture in children with the risk of obstructive sleep apnea. Int J Pediatr Otorhinolaryngol. 2021 May.
Koka V, De Vito A, Roisman G, Petitjean M, Filograna Pignatelli GR, Padovani D, Randerath W. Orofacial Myofunctional Therapy in Obstructive Sleep Apnea Syndrome: A Pathophysiological Perspective. Medicina (Kaunas). 2021 Apr 1;57(4):323.
Shah SS, Nankar MY, Bendgude VD, Shetty BR. Orofacial Myofunctional Therapy in Tongue Thrust Habit: A Narrative Review. Int J Clin Pediatr Dent. 2021 Mar-Apr;14(2):298-303.
Maspero C, Prevedello C, Giannini L, Galbiati G, Farronato G. Atypical swallowing: a review. Minerva Stomatol. 2014 Jun;63(6):217-27.
Tanny L, Huang B, Naung NY, Currie G. Non-orthodontic intervention and non-nutritive sucking behaviours: A literature review. Kaohsiung J Med Sci. 2018 Apr;34(4):215-222.
Alves GÂDS, Gondim YRDR, Lima JAS, Silva MAPD, Florêncio DSF, Almeida LNA, Silva HJD. Effects of photobiomodulation associated with orofacial myofactional therapy on temporomandibular joint dysfunction. Codas. 2021 Jun 4;33(6):e20200193.



